Community
Only other ostomates can truly understand exactly what it is like living with a stoma. People like you who often share the same underlying health conditions, who have recovered from surgery and are living their best life. If you need additional support you can reach out to local charities and associations in your community; they are often run by ostomates or can put you in touch with people who can help.
You can of course reach out to us at any time, we are here to help you find the support you need. Contact us on [email protected]
-
Support in the US

United Ostomy Associations of America, Inc. (UOAA) is a nonprofit organization that supports, empowers, and advocates for people who have had or who will have ostomy or continent diversion surgery.
Phone: 1-800-826-0826
P.O. Box 525, Kennebunk, ME 04043-0525
Information Line hours are Monday-Friday, 9AM to 3PM (Wednesday until 2PM) EST. If you have an emergency, please dial 911 or contact your local medical professional.
-
Support in Canada

Ostomy Canada Society is a non-profit volunteer organization dedicated to all people with an ostomy, and their families, helping them to live life to the fullest through support, education, collaboration and advocacy.
Phone: 1-905-212-7111
Toll Free Phone: 1-888-969-9698 (within Canada)
-
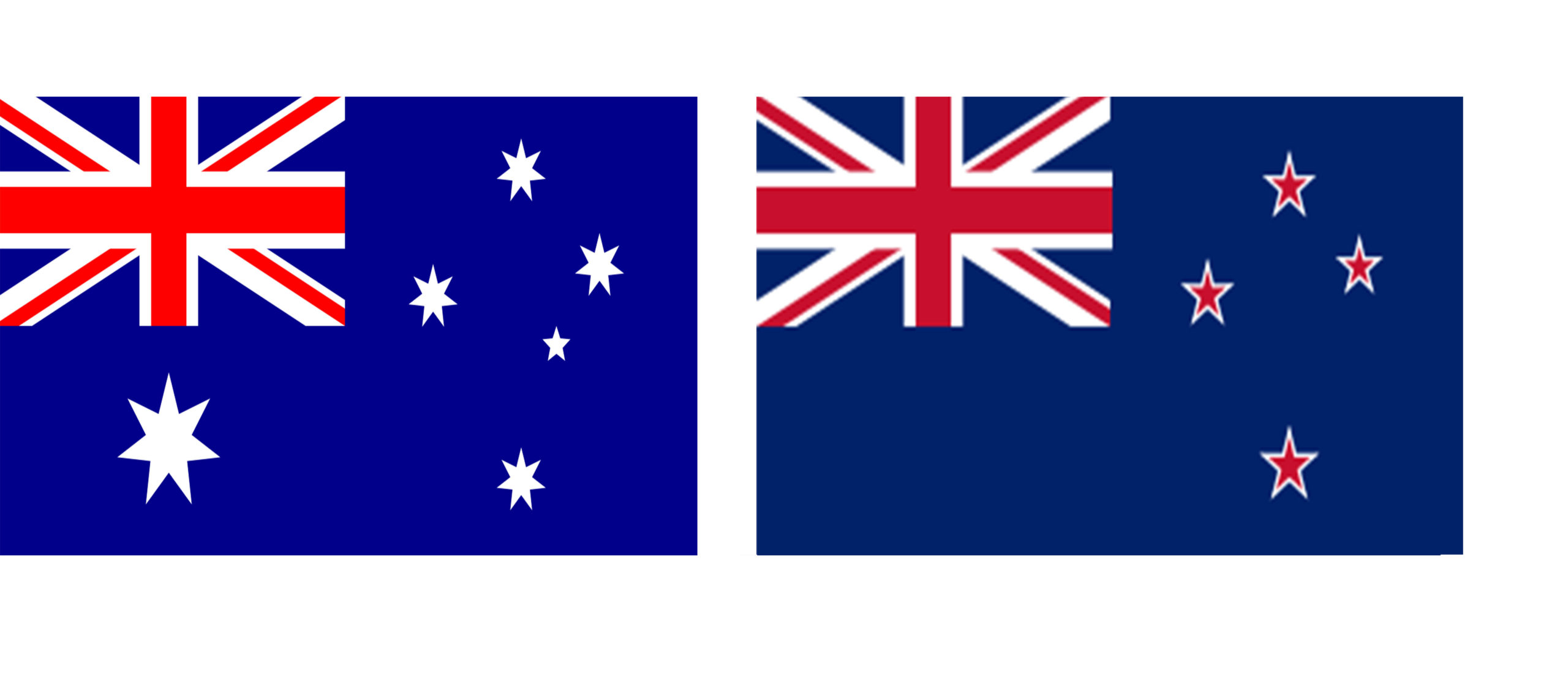
Support in Australia & New Zealand
The Australian Council of Stoma Associations Inc. (ACSA) is the National Body representing 21 ostomy associations and, through the membership of these associations, approximately 46,000 persons living with an ostomy throughout Australia.
www.australianstoma.com.au/associations
If you need stoma product support contact Omnigon, an independent, Australian owned company specialising in the supply of ostomy and wound care products to the Australian and New Zealand healthcare markets.
Australia
AUS Freecall 1800 819 274
AUS Freefax 1800 242 704
Email [email protected]New Zealand
PO Box 24139, Royal Oak Auckland 1345 New Zealand
NZ Freecall 0800 440 027
Email [email protected] -
Support in UK

If you would like advice on products and services to help with your stoma care routine please contact:
Tel: 0800 220 300
For advice on living with a stoma please contact one of the charities or associations below:
Colostomy Association
www.colostomyassociation.org.uk
Tel: 0118 939 1537 Helpline: 0800 328 4257The Urostomy Association
www.urostomyassociation.org.uk
Tel: 01386 430140The Ileostomy and Internal Pouch Support Group (IA)
www.iasupport.org
Tel: 0800 0184 724Other support groups and associations:
Macmillan Cancer Relief
www.macmillan.org.uk
Tel: 020 7840 7840Bowel Cancer UK
www.bowelcanceruk.org.ukTel: 0845 719300 or 020 7940 1760
Crohn’s & Colitis UK
http://www.crohnsandcolitis.org.uk/Tel: 0300 222 5700
-
Support in Republic of Ireland

Ostomy Associations of Ireland is a non-profit organization that supports people who have a stoma or internal pouch, or who are about to have surgery.
If you are looking for a local support group, please see our group page here, which lists all the active local groups.
All the groups have contact details. Please feel free to contact the group that you are interested in. The contact person, will be happy to give you details of meeting times, location and dates, for their specific group.
Do you have a story you want added to A Bigger Life?
Submit your own story and we will get back to you.



